 |
| A mosquito's spit can be worse than its bite alone. In some cases, the insect's saliva makes the viral disease dengue fever more severe. |
Mosquito saliva can increase dengue severity
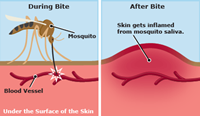
Insects transmit diseases when, probing for blood vessels, they inject saliva together with viral, bacterial, or parasitic pathogens into the skin of mammalian hosts. In mice, scientists found that mosquito spit weakened blood vessels, making them more permeable, or "leaky". Easier exchange between the blood and tissues may help the virus spread faster - and increase the severity of disease - immunologist Michael Schmid and colleagues report online June 16 in PLOS Pathogens. In tropical regions, Aedes mosquitoes transmit dengue virus (DENV) as well as other closely related viruses such as Zika. DENV infects almost 400 million humans every year. There are four types of DENV. They are referred to as serotypes 1-4 because, following infection, individuals have distinct antibody profiles in their blood serum, resulting from specific immune responses to each of the four virus types. DENV can cause severe disease, especially in people who have previously been exposed to a different serotype of the virus. In such patients, a phenomenon called "antibody-dependent enhancement" (ADE) takes place, during which antibodies that were generated during the first infection bind but do not destroy the slightly different newly infecting virus, but instead facilitate its infection of immune cells. The resulting higher viral burden in the patients causes more severe disease symptoms, or even death. Mosquito saliva is known to modulate transmission of some insect-borne pathogens and influence the host immune responses, but its role in dengue disease is not well understood. Investigating spit is important, says virologist Eva Harris of the University of California, Berkeley, a coauthor of the study. Molecules in mosquito saliva "can modify and modulate the infection process," she says. Saliva's role is well-studied in other viral diseases, like West Nile, but not for dengue. To investigate it, Michael Schmid and Eva Harris, from the University of California in Berkeley, USA, together with colleagues, studied mice inoculated with DENV alone, or with DENV plus extract from mosquito salivary glands. The researchers used mice that were susceptible to DENV infection via the skin and inoculated amounts of virus and saliva thought to resemble actual amounts transferred during a mosquito bite. Some of the mice were inoculated with antibodies binding to different DENV serotypes, whereas a second group was naive, that is, they did not have any anti-DENV antibodies. Among mice that had antibodies, i.e., during antibody-enhanced infection, the researchers found that the addition of saliva extract caused more severe disease than virus alone. In contrast, saliva extract did not influence disease severity and symptoms in na�ve mice. The researchers also report that saliva increased DENV infection of immune cells in the skin and enhanced immune cell migration to neighboring lymph nodes, which could promote the spread of disease throughout the body. They further observed that mosquito saliva increases the permeability (i.e., the leakiness) of endothelial cells that line blood vessels. They designed an experiment to examine permeability, and found that the presence of saliva allowed markers to leak out of the blood vessels at the injection site and into the surrounding tissue in the ear. The same is presumably true for DENV infection in the presence of mosquito saliva. Salivary gland extract enhances permeability of blood vessels in the mouse ear as indicated by the wider spread of the red marker (top) compared to an untreated ear (bottom). Credit: Michael A. Schmid and Dustin R. Glasner; CCAL |
In a final set of experiments, the researchers removed the skin surrounding the site of transmission shortly after inoculation. This prevented severe disease following antibody-enhanced infection when only virus was inoculated, but the protective effect of the operation was lost when saliva was also present. This suggests that mosquito saliva promotes the faster and/or wider spread of virus from the injection site.
The researchers speculate that, "via disruption of endothelial barrier function in the skin, mosquito salivary gland extract may augment access of DENV to enhancing antibodies in the serum, increase the spread of infectious virus-antibody complexes, enhance infection within systemic tissues, and thus exacerbate dengue pathogenesis during ADE." Based on their findings, they urge that "mosquito saliva and enhancing antibodies thus need to be considered when developing vaccines and drugs against dengue," and specifically suggest that "animal models of dengue and pre-clinical validation of dengue vaccine candidates should be evaluated in the combined presence of mosquito saliva and enhancing antibodies." These results should be interpreted with caution, says Duane Gubler, an infectious disease researcher at Duke University who was not involved in the study. Various environmental and genetic factors also play a role in the severity of the disease. "It's not clear-cut," he says. More broadly, the researchers call "for additional research on arthropod-borne pathogens whose vectors share similar blood-feeding strategies and may also impair endothelial barrier function."
Journal Reference: 1. Michael A. Schmid, Dustin R. Glasner, Sanjana Shah, Daniela Michlmayr, Laura D. Kramer, Eva Harris. Mosquito Saliva Increases Endothelial Permeability in the Skin, Immune Cell Migration, and Dengue Pathogenesis during Antibody-Dependent Enhancement. PLOS Pathogens, 2016; 12 (6): e1005676 DOI:10.1371/journal.ppat.1005676
|

