|
Tổng hợp các nghiên cứu sâu về nhiễm ký sinh trùng cơ hội trên bệnh nhân suy giảm miễn dịch
Thuật ngữ suy giảm miễn dịch theo tiếng Anh gồm Immunodeficiency, hoặc Immune deficiency. Theo phân loại bệnh tật quốc tế là ICD-10 (D84.9), ICD-9M (279.3), DiseasesDB (21506) vàMeSHD (007153). Trong đó, suy giảm miễn dịch (SGMD) là tình trạng khả năng hệ miễn dịch chống lại các bệnh nhiễm trùng và ung thư bị suy giảm hay mất hoàn toàn. SGMD gồm có hai loại: SGMD thứ phát: do yếu tố nội-ngoại sinh ảnh hưởng lên hệ thống miễn dịch, gồm nhiễm trùng HIV, tuổi cao, môi trường, dinh dưỡng, thuốc ức chế miễn dịch, ghép tạng, bệnh tự miễn, tiểu đường, lao, hội chứng chuyển hóa nặng;SGMD tiên phát: trẻ sinh ra đã khiếm khuyết miễn dịch; Một người SGMD bất kỳ loại nào dễ dẫn đến nhiễm trùng cơ hội (opportunistic infection) trên nền các nhiễm trùng bình thường. SGMD thể dịch gồm có rối loạn chức năng tế bào B với các triệu chứng lệ thuộc nguyên nhân. Nếu giảm gammaglobuline máu (Ab), kèm nhiễm trùng hô hấp tái lại, hay mất gammaglobulin (thiếu sinh Ab) à nhiễm trùng nặng và cuối cùng là tử vong. SGMD tế bào T dẫn đến rối loạn thứ phát như SGMD mắc phải AIDS. Nếu giảm hoặc mất bạch cầu hạt (đặc biệt là bạch cầu đa nhân trung tính), giảm cả số lượng và chức năng. Một số khác là suy giảm chức năng tạng lách, suy giảm các thành phần trong hệ thống bổ thể và SGMD thường tác động lên nhiều thành phần bổ thể. 
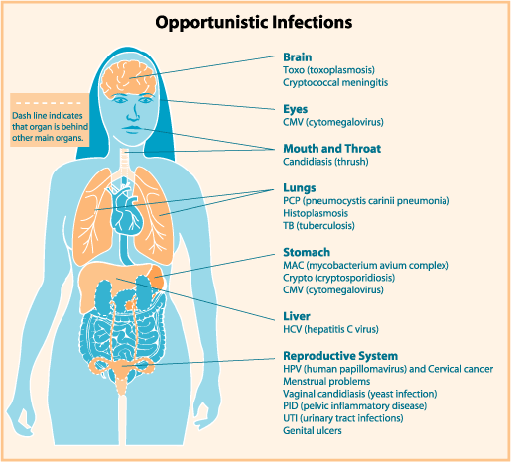
Hình 1
1.UNAIDS report on the global AIDS epidemic 2010. Epidemic update. [accessed on August 25, 2011]. Available from: http://www.unaids.org/documents/GlobalReport_Chap2_em.pdf 2.CDC. Revision of the CDC surveillance case definition for acquired immunodeficiency syndrome. MMWR Surveill Summ. 1987;36:1-15. [PubMed] 3.Akinbo FO, Okaka CE, Omoregie R. Prevalence of intestinal parasitic infections among HIV patients in Benin City, Nigeria. 2010; 5 -doi: 10. Libyan J Med. 2010;5 doi: 10.3402/ljm.v5i0.5506. [PMC free article][PubMed] 4.Mohandas, Sehgal R, Sud A, Malla N. Prevalence of intestinal parasitic pathogens in HIV-seropositive individuals in Northern India. Jpn J Infect Dis.2002;55:83-4. [PubMed] 5.Fontanet AL, Sahlu T, Rinke de Wit T, Messele T, Masho W, Woldemichael T, et al. Epidemiology of infections with intestinal parasites and human immunodeficiency virus (HIV) among sugar-estate residents in Ethiopia. Ann Trop Med Parasitol. 2000;94:269-78. [PubMed] 6.Lindo JF, Dubon JM, Ager AL, de Gourville EM, Solo-Gabriele H, Klaskala WI, et al. Intestinal parasitic infections in human immunodeficiency virus (HIV)-positive and HIV-negative individuals in San Pedro Sula, Honduras. Am J Trop Med Hyg. 1998;58:431–5. [PubMed] 7.Omalu ICJ, Yako AB, Duhlinska DD, Anyanwu GI, Pam VA, Inyama PU. First detection of intestinal microsporidia in Nigeria. Online J Health All Sci. 2005;3:4. 8.Kulkarni SV, Kairon R, Sane SS, Padmawar PS, Kale VA, Thakar MR, et al. Opportunistic parasitic infections in HIV/AIDS patients presenting with diarrhoea by the level of immunesuppression. Indian J Med Res. 2009;131:63-6. [PubMed] 9.Asma I, Johari S, Sim BHL, Lim YAL. How common is intestinal parasitism in HIV-infected patients in Malaysia? Trop Biomed. 2011;28:400-10. [PubMed] 10.Siddiqui U, Bini EJ, Chandarana K, Leong J, Ramsetty S, Schiliro D, et al. Pravalence and impact of diarrhea on health-related quality of life in HIV-infected patients in the era of highly active antiretroviral therapy. J Clin Gastroenterol. 2007;41:484-90. [PubMed] 11.Lagrange-Xélot M, Porcher R, Sarfati C, de Castro N, Carel O, Magnier JD, et al. Isosporiasis in patients with HIV infection in the highly active antiretroviral therapy era in France. HIV Med. 2008;9:126-30. [PubMed] 12.Chhin S, Harwell JI, Bell JD, Rozycki G, Ellman T, Barnett JM, et al. Etiology of chronic diarrhea in antiretroviral-naive patients with HIV infection admitted to Norodom Sihanouk Hospital, Phnom Penh, Cambodia. Clin Infect Dis. 2006;43:925-32. [PubMed] 13.Kosek M, Alcantara C, Lima AA, Guerrant RL. Cryptosporidiosis: an update. Lancet Infect Dis. 2001;1:262-9. [PubMed] 14.Wiwanitkit V. Intestinal parasitic infections in Thai HIV-infected patients with different immunity status. BMC Gastroenterol. 2001;1:3. [PMC free article][PubMed] 15.Leelayoova S, Vithayasai N, Watanaveeradej V, Chotpitayasunondh T, Therapong V, Naaglor T, et al. Intestinal microsporidiosis in HIV-infected children with acute and chronic diarrhea. Southeast Asian J Trop Med Public Health. 2001;32:33-7. [PubMed] 16.Wanachiwanawin D, Chokephaibulkit K, Lertlaituan P, ongrotchanakun J, Chinabut P, Thakerngpol K. Intestinal microsporidiosis in HIV-infected children with diarrhea. Southeast Asian J Trop Med Public Health. 2002;33:241-5. [PubMed] 17.Sokolova OI, Demyanov AV, Bowers LC, Didier ES, Yakovlev AV, Skarlato SO, et al. Emerging microsporidian infections in Russian HIV-infected patients. J Clin Microbiol. 2011;49:2102-8. [PMC free article][PubMed] 18.Didier ES, Weiss LM. Microsporidiosis: Not just in AIDS patients. Curr Opin Infect Dis.2011;24:490-5. [PMC free article][PubMed] 19.Stauffer W, Radvin JI. Entamoeba histolytica: an update. Curr Opin Infect Dis. 2003;16:479-85. [PubMed] 20.Haque R, Huston CD, Hughes M, Houpt E, Petri WA. Amebiasis. N Engl J Med. 2003;348:1565-73. [PubMed] 21.Hung CC, Wu PY, Chang SY, Ji DD, Sun HY, Liu WC, et al. Amebiasis among persons who sought voluntary counseling and testing for human immunodeficiency virus infection: a case-control study. Am J Trop Med Hyg. 2011;84:65-9. [PMC free article][PubMed] 22.Chen Y, Zhang Y, Yang B, Qi T, Lu H, Cheng X, et al. Seroprevalence of Entamoeba histolytica infection in HIV-Infected patients in China. Am J Trop Med Hyg. 2007;77:825–8. [PubMed] 23.Hung CC, Wu PY, Chang SY, Ji DD, Sun HY, Liu WC, et al. Amebiasis among persons who sought voluntary counseling and testing for human immunodeficiency virus infection: a case control study. Am J Trop Med Hyg. 2011;84:65-9. [PMC free article][PubMed] 24.Lee YJ, Chen KJ, Yang CH, Lin YC, Liu HY, Liao ST, et al. Characteristics of amebic liver abscess in patients with or without human immunodeficiency virus. J Microbiol Immunol Infect. 2009;42:500–4. [PubMed] 25.Wu KS, Tsai HC, Lee SS, Liu YC, Wann SR, Wang YH, et al. Comparison of clinical characteristics of amebic liver abscess in human immunodeficiency virus (HIV)-infected and non-HIV-infected patients. J Microbiol Immunol Infect. 2008;41:456–61. [PubMed] 26.Feitosa G, Bandeira AC, Sampaio DP, Badaró R, Brites C. High prevalence of giardiasis and stronglyloidiasis among HIV-infected patients in Bahia, Brazil. Braz J Infect Dis. 2001;5:339-44. [PubMed] 27.Chui DW, Owen RL. AIDS and the gut. J Gastroenterol Hepatol. 1994;9:291–303. [PubMed] 28.Hailemariam G, Kassu A, Abebe G, Abate E, Damte D, Mekonnen E, et al. Intestinal parasitic infections in HIV/AIDS and HIV seronegative individuals in a teaching hospital, Ethiopia. Jpn J Infect Dis. 2004;57:41–3. [PubMed]. 29.Angarano G, Maggi P, Di Bari MA, Larocca AM, Congedo P, Di Bari C, et al. Giardiasis in HIV: A possible role in patients with severe immune deficiency. Eur J Epidemiol. 1997;13:485–7. [PubMed] 30.Phillips MA, Stanley SL., Jr . Chemotherapy of protozoal infections: Amebiasis, giardiasis, trichomoniasis, trypanosomiasis, leishmaniasis, and other protozoal infections. In: Brunton LL, Chabner BA, Knollman BC, editors. Goodman & Gilman's the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill; 2001. 31.Fujishima T, Nishise S, Ichihara M, Kobayashi S, Takeuchi T. Difficulties in the treatment of intestinal amoebiasis in mentally disabled individuals at a rehabilitation institution for the intellectually impaired in Japan. Chemotherapy. 2010;56:348–52. [PubMed] 32.Wiwanitkit V, Srisupanant M. Cryptosporidiosis occurrence in anti-HIV-seropositive patients attending a sexually transmitted diseases clinic, Thailand. Trop Doct. 2006;36:64. [PubMed] 33.WHO. Control of the leishmaniases. WHO Technical Report Series.2010;949:1-104. 34.Alvar J, Bashaye S, Argaw D, Cruz I, Aparicio P, Kassa A, et al. Kala-azar outbreak in Libo Kemkem, Ethiopia: epidemiologic and parasitologic assessment. Am J Trop Med Hyg. 2007;77:275–82. [PubMed] 35.Alvar J, Aparicio P, Aseffa A, Den Boer M, Cañavate C, Dedet JP, et al. The relationship between leishmaniasis and AIDS: the second 10 years. Clin Microbiol Rev. 2008;21:334-59. [PMC free article][PubMed] 36.Reithinger R, Dujardin JC, Louzir H, Pirmez C, Alexander B, Brooker S. Cutaneous leishmaniasis. Lancet Infect Dis. 2007;7:581-96. [PubMed] 37.Paredes R, Munoz J, Diaz I, Domingo P, Gurgui M, Clotet B. Leishmaniasis in HIV infection. J Postgrad Med. 2003;49:39-49. [PubMed] 38.Guiguemdé RT, Sawadogo OS, Bories C, Traore KL, Nezien D, Nikiema L, et al. Leishmania major and HIV co-infection in Burkina Faso. Trans R Soc Trop Med Hyg. 2003;97:168-9. [PubMed] 39.Rabello A, Orsini M, Disch J. Leishmania/HIV co-infection in Brazil: an appraisal. Ann Trop Med Parasitol.2003;97(Suppl 1):17-28. [PubMed] 40.Chakravarty J, Kumar S, Kumar R, Gautam S, Rai M, Sundar S. Evaluation of rk39 immunochromatographic test with urine for diagnosis of visceral leishmaniasis. Trans R Soc Trop Med Hyg. 2011;105:537-9. [PMC free article][PubMed]. 41.Desjeux P. Global control and Leishmania HIV co-infection. Clin Dermatol.1999;17:317-25. [PubMed] 42.Calza L, D’Antuono A, Marinacci G, Manfredi R, Colangeli V, Passarini B, et al. Disseminated cutaneous leishmaniasis after visceral disease in a patient with AIDS. J Am Acad Dermatol.2004;50:461-5. [PubMed] 43.Schönian G, Nasereddin A, Dinse N, Schweynoch C, Schallig HD, Presber W, et al. PCR diagnosis and characterization of Leishmania in local and imported clinical samples. Diagn Microbiol Infect Dis.2003;47:349–58. [PubMed] 44.Antinori S, Longhi E, Bestetti G, Piolini R, Acquaviva V, Foschi A, et al. Post-kala-azar dermal leishmaniasis as an immune reconstitution inflammatory syndrome in a patient with acquired immune deficiency syndrome. Br J Dermatol.2007;157:1032–6. [PubMed]. 45.Ritmeijer K, Veeken H, Melaku Y, Leal G, Amsalu R, Seaman J, et al. Ethiopian visceral leishmaniasis: generic and proprietary sodium stibogluconate are equivalent; HIV co-infected patients have a poor outcome. Trans R Soc Trop Med Hyg.2001;95:668-72. [PubMed] 46.Rosenthal E, Marty P. Recent understanding in the treatment of visceral leishmaniasis. J Postgrad Med. 2003;49:61-8. [PubMed] 47.Davidson RN, Russo R. Relapse of visceral leishmaniasis in patients who were coinfected with human immunodeficiency virus and who received treatment with liposomal amphotericin B. Clin Infect Dis.1994;19:560. [PubMed] 48.WHO 2009. Reported malaria cases and deaths [cited 2011 Aug 25] [accessed on August 25, 2011]. Available from: http://www.who.int/malaria/world_malaria_report.pdf . 49.Idemyor V. Human immunodeficiency virus (HIV) and malaria interaction in sub-Saharan Africa: the collision of two Titans. HIV Clin Trials.2007;8:246–53. [PubMed] 50.Cruciani M, Nardi S, Malena M, Bosco O, Serpelloni G, Mengoli C. Systematic review of the accuracy of the ParaSight-F test in the diagnosis of Plasmodium falciparum malaria. Med Sci Monit. 2004;10:MT81–8. [PubMed] 51.Patankar TF, Karnad DR, Shetty PG, Desai AP, Prasad SR. Adult cerebral malaria: prognostic importance of imaging findings and correlation with postmortem findings. Radiology.2002;224:811-6. [PubMed] 52.Cordoliani YS, Sarrazin JL, Felten D, Caumes E, Lévêque C, Fisch A. MR of cerebral malaria. AJNR Am J Neuroradiol. 1998;19:871–4. [PubMed] 53.Mohsen AH, McKendrick MW, Schmid ML, Green ST, Hadjivassiliou M, Romanowski C. Postmalaria neurological syndrome: a case of acute disseminated encephalomyelitis? J Neurol Neurosurg Psychiatry.2000;68:388-9. [PMC free article][PubMed] 54.WHO. 2008. Essential prevention and care interventions for adults and adolescents living with HIV in resource-limited settings. [accessed on December 6, 2011]. Available from: http://www.who.int/hiv/pub/prev_care/OMS_EPP_AFF_en.pdf . 55.Garcia HH, Pretell J, Gilman RH Cysticercosis Working Group in Peru. Neurocysticercosis and the global world. J Neurol. 2002;249:1107–8. [PubMed] 56.Garcia HH, Del Brutto OH Cysticercosis Working Group in Peru. Neurocysticercosis: updated concepts about an old disease. Lancet Neurol.2005;4:653-61. [PubMed] 57.Walker M, Zunt JR. Parasitic central nervous system infections in immunocompromised hosts. Clin Infect Dis.2005;40:1005-15. [PMC free article][PubMed] 58.Takayanagui OM, Odashima NS, Bonato PS, Lima JE, Lanchote VL. Medical management of neurocysticercosis. Expert Opin Pharmacother. 2011;12:2845-56. [PubMed] 59.WHO Expert Committee. Prevention and control of schistosomiasis and soil-transmitted helminthiasis. (1-57).World Health Organ Tech Rep Ser. 2002;912:i–vi. [PubMed] 60.Ross AG, Bartley PB, Sleigh AC, Olds GR, Li Y, Williams GM, et al. Schistosomiasis. N Engl J Med. 2002;346:1212-20. [PubMed] 61.Smith C, Smith H, Seaton RA, Fox R. Seroprevalence of schistosomiasis in African patients infected with HIV. HIV Med. 2008;9:436–9. [PubMed] 62.de Avila RE, Batista TS, Xavier MA, Nogueira AM, Lambertucci JR. Schistosomiasis mansoni and severe gastrointestinal cytomegalovirus disease in a patient with acquired immunodeficiency syndrome. Rev Soc Bras Med Trop. 2006;39:379–82. [PubMed] 63.Carod-Artal FJ. Neuroschistosomiasis. Expert Rev Anti Infect Ther.2010;8:1307–18. [PubMed] 64.Carod-Artal FJ. Neurological complications of Schistosoma infection. Trans R Soc Trop Med Hyg.2008;102:107-16. [PubMed] 65.Ferrari TC. Involvement of central nervous system in the schistosomiasis. Mem Inst Oswaldo Cruz. 2004;99(5 Suppl 1):59-62. [PubMed] 66.Zhu YC. Immunodiagnosis and its role in schistosomiasis control in China: A review. Acta Trop. 2005;96:130-6. [PubMed] 67.Van Gool T, Vetter H, Vervoort T, Doenhoff MJ, Wetsteyn J, Overbosch D. Serodiagnosis of imported schistosomiasis by a combination of a commercial indirect hemagglutination test with Schistosoma mansoni adult worm antigens and an enzyme-linked immunosorbent assay with S. mansoni egg antigens. J Clin Microbiol. 2002;40:3432-7. [PMC free article][PubMed] 68.Fowler R, Lee C, Keystone JS. The role of corticosteroids in the treatment of cerebral schistosomiasis caused by Schistosoma mansoni: case report and discussion. Am J Trop Med Hyg.1999;61:47-50. [PubMed] 69.Liu HQ, Feng XY, Yao ZW, Sun HP. Characteristic magnetic resonance enhancement pattern in cerebral schistosomiasis. Chin Med Sci J.2006;21:223-7. [PubMed] 70.Ferrari ML, Coelho PM, Antunes CM, Tavares CA, da Cunha AS. Efficacy of oxamniquine and praziquantel in the treatment of Schistosoma mansoni infection: a controlled trial. Bull World Health Organ. 2003;81:190-6. [PMC free article][PubMed] 71.Xiao SH, You JQ, Gao HF, Mei JY, Jiao PY, Chollet J, et al. Schistosoma japonicum: effect of artemether on glutathione S-transferase and superoxide dismutase. Exp Parasitol. 2002;102:38–45. [PubMed] 72.Karanja DM, Hightower AW, Colley DG, Mwinzi PN, Galil K, Andove J, et al. Resistance to reinfection with Schistosoma mansoni in occupationally exposed adults and effect of HIV-1 co-infection on susceptibility to schistosomiasis: a longitudinal study. Lancet. 2002;360:592–6. [PubMed] 73.Rivero FD, Kremer LE, Allende L, Casero RD. Strongyloides stercoralis and HIV: a case report of an indigenous disseminated infection from non-endemic area. Rev Argent Microbiol.2006;38:137-9. [PubMed] 74.Viney ME, Brown M, Omoding NE, Bailey JW, Gardner MP, Roberts E, et al. Why does HIV infection not lead to disseminated strongyloidiasis? J Infect Dis.2004;190:2175-80. [PubMed] 75.Keiser PB, Nutman TB. Strongyloides stercoralis in the Immunocompromised Population. Clin Microbiol Rev. 2004;17:208-17. [PMC free article][PubMed] 76.Walker MD, Zunt JR. Neuroparasitic infections: Nematodes. Semin Neurol. 2005;25:252–61. [PMC free article][PubMed] 77.Siddiqui AA, Berk SL. Diagnosis of Strongyloides stercoralis infection. Clin Infect Dis. 2001;33:1040-7. [PubMed] 78.Nissapatorn V, Lee C, Quek KF, Leong CL, Mahmud R, Abdullah KA. Toxoplasmosis in HIV/AIDS patients: a current situation. Jpn J Infect Dis. 2004;57:160–5. [PubMed] 79.Israeski DM, Remington JS. AIDS-associated toxoplasmosis. In: Sande MA, Volberding PA, editors. The medical management of AIDS. Philadelphia: WB Saunders; 1992. pp. 319–45. 80.Carme B, M’Pele P, Mbitsi A, Kissila AM, Aya GM, Mouanga-Yidika G, et al. Opportunistic parasitic diseases and mycoses in AIDS.Their frequencies in Brazzaville (Congo) Bull Soc Pathol Exot Filiales.1988;81:311-6. [PubMed] 81.Colombo FA, Vidal JE, Penalva de Oliveira AC, Hernandez AV, Bonasser-Filho F, Nogueira RS, et al. Diagnosis of cerebral toxoplasmosis in AIDS patients in Brazil: importance of molecular and immunological methods using peripheral blood samples. J Clin Microbiol.2005;43:5044-7. [PMC free article][PubMed] 82.Vidal JE, Hernandez AV, de Oliveira AC, Dauar RF, Barbosa SP, Jr, Focaccia R. Cerebral toxoplasmosis in HIV-positive patients in Brazil: clinical features and predictors of treatment response in the HAART era. AIDS Patient Care STDS. 2005;19:626-34. [PubMed] 83.Pereira-Chioccola VL, Vidal JE, Su C. Toxoplasma gondii infection and cerebral toxoplasmosis in HIV-infected patients. Future Microbiol. 2009;4:1363-79. [PubMed] 84.Luft BJ. Toxoplasma gondii. In: Walzer PD, Gertz R, editors. Parasitic infection in the compromised host. New York: Marcel Dekker; 1989. pp. 179-279. 85.Luft BJ, Remington JS. Toxoplasmic encephalitis in AIDS. Clin Infect Dis. 1992;15:211–22. [PubMed] 86.Reischl U, Bretagne S, Krüger D, Ernault P, Costa JM. Comparison of two DNA targets for the diagnosis of Toxoplasmosis by real-time PCR using fluorescence resonance energy transfer hybridization probes. BMC Infect Dis. 2003;3:7. [PMC free article][PubMed] 87.Antinori A. Evaluation and management of intracranial mass lesions in AIDS: Report of the Quality Standard Subcommittee of the American Academy of Neurology. Neurology. 1998;51:1233-4. [PubMed] 88.Yeo KK, Yeo TT, Chan CY, Sitoh YY, Teo J, Wong SY. Stereotactic brain biopsies in AIDS patients-early local experience. Singapore Med J. 2000;41:161–6. [PubMed] 89.Sadler M, Brink NS, Gazzard BG. Management of intracerebral lesions in patients with HIV: a retrospective study with discussion of diagnostic problems. QJM. 1998;91:205–17. [PubMed] 90.Armbruster C, Alesch F, Budka H, Kriwanek S. Stereotactic brain biopsy in AIDS patients: a necessary patient-oriented and cost-effective diagnostic measure? Acta Med Austriaca. 1998;25:91-5. [PubMed] 91.Cota GF, Assad EC, Christo PP, Giannetti AV, Santos Filho JA, Xavier MA. Ventriculitis: a rare case of primary cerebral toxoplasmosis in AIDS patient and literature review. Braz J Infect Dis. 2008;12:101–4. [PubMed] 92.Portegies P, Solod L, Cinque P, Chaudhuri A, Begovac J, Everall I, et al. Guidelines for the diagnosis and management of neurological complications of HIV infection. Eur J Neurol. 2004;11:297–304. [PubMed] 93.Kung DH, Hubenthal EA, Kwan JY, Shelburne SA, Goodman JC, Kass JS. Toxoplasmosis myelopathy and myopathy in an AIDS patient: a case of immune reconstitution inflammatory syndrome? Neurologist. 2011;17:49–51. [PubMed] 94.Chirgwin K, Hafner R, Leport C, Remington J, Andersen J, Bosler EM, et al. Randomized phase II trial of atovaquone with pyrimethamine or sulfadiazine for treatment of toxoplasmic encephalitis in patients with acquired immunodeficiency syndrome: ACTG 237/ANRS 039 Study. AIDS Clinical Trials Group 237/Agence Nationale de Recherche sur le SIDA, Essai 039. Clin Infect Dis. 2002;34:1243–50. [PubMed] 95.Baggish AL, Hill DR. Antiparasitic agent atovaquone. Antimicrob Agents Chemother. 2002;46:1163–73. [PMC free article][PubMed] 96.Coura JR. Chagas disease: what is known and what is needed--a background article. Mem Inst Oswaldo Cruz. 2007;102(Suppl 1):113–22. [PubMed] 97.Jackson Y, Myers C, Diana A, Marti HP, Wolff H, Chappuis F, et al. Congenital transmission of Chagas disease in Latin American immigrants in Switzerland. Emerg Infect Dis. 2009;15:601–3. [PMC free article][PubMed] 98.Vaidian AK, Weiss LM, Tanowitz HB. Chagas’ disease and AIDS. Kinetoplastid Biol Dis. 2004;3:2. [PMC free article][PubMed] 99.Antunes AC, Cecchini FM, Bolli FB, Oliveira PP, Reboucas RG, Monte TL, et al. Cerebral trypanosomiasis and AIDS. Arq Neuropsiquiatr. 2002;60:730–3. [PubMed] 100.Sica RE, Gargiullo G, Papayanis C. Tumour-like chagasic encephalitis in AIDS patients: an atypical presentation in one of them and outcome in a small series of cases. Arq Neuropsiquiatr. 2008;66:881–4. [PubMed] 101.Madalosso G, Pellini AC, Vasconcelos MJ, Ribeiro AF, Weissmann L, Oliveira Filho GS, et al. Chagasic meningoencephalitis: case report of a recently included AIDS-defining illness in Brazil. Rev Inst Med Trop Sao Paulo. 2004;46:199–202. [PubMed] 102.Cordova E, Boschi A, Ambrosioni J, Cudos C, Corti M. Reactivation of Chagas disease with central nervous system involvement in HIV-infected patients in Argentina, 1992-2007. Int J Infect Dis. 2008;12:587–92. [PubMed] 103.Ferreira MS, Borges AS. Some aspects of protozoan infections in immunocompromised patients - a review. Mem Inst Oswaldo Cruz. 2002;97:443–57. [PubMed] 104.DiazGranados CA, Saavedra-Trujillo CH, Mantilla M, Valderrama SL, Alquichire C, Franco-Paredes C. Chagasic encephalitis in HIV patients: common presentation of an evolving epidemiological and clinical association. Lancet Infect Dis. 2009;9:324-30. [PubMed] 105.Burgos JM, Begher SB, Freitas JM, Bisio M, Duffy T, Altcheh J, et al. Molecular diagnosis and typing of Trypanosoma cruzi populations and lineages in cerebral Chagas disease in a patient with AIDS. Am J Trop Med Hyg. 2005;73:1016–8. [PubMed] 106.Pittella JE. Central nervous system involvement in Chagas disease: a hundred-year-old history. Trans R Soc Trop Med Hyg. 2009;103:973–8. [PubMed] 107.Montero A, Cohen JE, Martínez DP, Giovannoni AG. Empirical anti-toxoplasma therapy in cerebral AIDS and Chagas disease. Presentation of 2 cases, review of the literature and proposal of an algorithm. Medicina (B Aires) 1998;58:504–6. [PubMed] 108.Corti M. AIDS and Chagas’ disease. AIDS Patient Care STDS. 2000;14:581–8. [PubMed] 109.Barratt JL, Harkness J, Marriott D, Ellis JT, Stark D. Importance of nonenteric protozoan infections in immunocompromised people. Clin Microbiol Rev. 2010;23:795–836. [PMC free article][PubMed] 110.Maldonado C, Albano S, Vettorazzi L, Salomone O, Zlocowski JC, Abiega C, et al. Using polymerase chain reaction in early diagnosis of re-activated Trypanosoma cruzi infection after heart transplantation. J Heart Lung Transplant.2004;23:1345-8. [PubMed] 111.Diez M, Favaloro L, Bertolotti A, Burgos JM, Vigliano C, Lastra MP, et al. Usefulness of PCR strategies for early diagnosis of Chagas’ disease reactivation and treatment follow-up in heart transplantation. Am J Transplant.2007;7:1633-40. [PubMed] 112.Piron M, Fisa R, Casamitjana N, López-Chejade P, Puig L, Vergés M, et al. Development of a real-time PCR assay for Trypanosoma cruzi detection in blood samples. Acta Trop.2007;103:195-200. [PubMed] 113.Corti M, Yampolsky C. Prolonged survival and immune reconstitution after chagasic meningoencephalitis in a patient with acquired immunodeficiency syndrome. Rev Soc Bras Med Trop. 2006;39:85-8. [PubMed] 114.Sartori AM, Caiaffa-Filho HH, Bezerra RC, do S Guilherme C, Lopes MH, Shikanai-Yasuda MA. Exacerbation of HIV viral load simultaneous with asymptomatic reactivation of chronic Chagas’ disease. Am J Trop Med Hyg.2002;67:521-3. [PubMed] 115.Kennedy PG. The continuing problem of human African trypanosomiasis (sleeping sickness) Ann Neurol.2008;64:116-26. [PubMed] 116.Barat C, Pepin J, Tremblay MJ. HIV-1 replication in monocyte-derived dendritic cells is stimulated by melarsoprol, one of the main drugs against human African trypanosomiasis. J Mol Biol. 2011;410:1052-64. [PubMed] 117.Laboratory diagnosis of parasites of public health concern. Atlanta, GA: CDC; 2003. CDC. 118.Lejon V, Boelaert M, Jannin J, Moore A, Büscher P. The challenge of Trypanosoma brucei gambiense sleeping sickness diagnosis outside Africa. Lancet Infect Dis. 2003;3:804–8. [PubMed] 119.Lejon V, Buscher P. Stage determination and follow-up in sleeping sickness. Med Trop (Mars) 2001;61:355–60. [PubMed] 120.Kennedy PG. Human African trypanosomiasis of the CNS: current issues and challenges. J Clin Invest. 2004;113:496–504. [PMC free article][PubMed] 121.Gill DS, Chatha DS, del Carpio-O’Donovan R. MR imaging findings in African trypansomiasis. AJNR Am J Neuroradiol. 2003;24:1383–5. [PubMed] 122.Matovu E, Seebeck T, Enyaru JC, Kaminsky R. Drug resistance in Trypanosoma brucei spp., the causative agents of sleeping sickness in man and nagana in cattle. Microbes Infect. 2001;3:763–70. [PubMed] 123.Docampo R, Moreno SN. Current chemotherapy of human African trypanosomiasis. Parasitol Res. 2003;90(Supp 1):S10–3. [PubMed] 124.Bouteille B, Oukem O, Bisser S, Dumas M. Treatment perspectives for human African trypanosomiasis. Fundam Clin Pharmacol. 2003;17:171–81. [PubMed] 125.Nok AJ. Arsenicals (melarsoprol), pentamidine and suramin in the treatment of human African trypanosomiasis. Parasitol Res. 2003;90:71–9. [PubMed] 126.Blum J, Nkunku S, Burri C. Clinical description of encephalopathic syndromes and risk factors for their occurrence and outcome during melarsopol treatment of human African trypanosomiasis. Trop Med Int Health. 2001;6:390–400. [PubMed] 127.de La Rosa R, Pineda JA, Delgado J, Macías J, Morillas F, Mira JA, et al. Incidence of and risk factors for symptomatic visceral leishmaniasis among human immunodeficiency virus type 1-infected patients from Spain in the era of highly active antiretroviral therapy. J Clin Microbiol. 2002;40:762–7. [PMC free article][PubMed] 128.Lian YL, Heng BS, Nissapatorn V, Lee C. AIDS-defining illnesses: a comparison between before and after commencement of highly active antiretroviral therapy (HAART) Curr HIV Res. 2007;5:484–9. [PubMed] 129.Silva MT, Araújo A. Highly active antiretroviral therapy access and neurological complications of human immunodeficiency virus infection: impact versus resources in Brazil. J Neurovirol. 2005;11(Suppl 3):11–5. [PubMed] 130.Tsambiras PE, Larkin JA, Houston SH. Case report.Toxoplasma encephalitis after initiation of HAART. AIDS Read. 2001;11:608-10. [PubMed] 131.de Boer J, Wulffraat N, Rothova A. Visual loss in uveitis of childhood. Br J Ophthalmol. 2003;87:879-84. [PMC free article][PubMed] 132.Sendi P, Sachers F, Drechsler H, Graber P. Immune recovery vitritis in an HIV patient with isolated toxoplasmic retinochoroiditis. AIDS. 2006;20:2237-8. [PubMed] 133.Chen KC, Chen JY, Tung GA. Case 149: Immune reconstitution inflammatory syndrome. Radiology. 2009;252:924–8. [PubMed] 134.Caby F, Lemercier D, Coulomb A, Grigorescu R, Paris L, Touafek F, et al. Fetal death as a result of placental immune reconstitution inflammatory syndrome. J Infect. 2010;61:185–8. [PubMed] 135.Belanger F, Derouin F, Grangeot-Keros L, Meyer L. Incidence and risk factors of toxoplasmosis in a cohort of human immunodeficiency virus-infected patients: 1988-1995. HEMOCO and SEROCO Study Groups. Clin Infect Dis. 1999;28:575–81. [PubMed] 136.Ullum H, Victor J, Katzenstein TL, Gerstoft J, Gøtzsche PC, Bendtzen K, et al. Decreased short-term production of tumor necrosis factor-alpha and interleukin-1beta in human immunodeficiency virus-seropositive subjects. J Infect Dis. 1997;175:1507–10. [PubMed] 137.Jevtović DJ, Salemović D, Ranin J, Pesić I, Zerjav S, Djurković-Djaković O. The prevalence and risk of immune restoration disease in HIV-infected patients treated with highly active antiretroviral therapy. HIV Med. 2005;6:140–3. [PubMed] 138.Furco A, Carmagnat M, Chevret S, Garin YJ, Pavie J, De Castro N, et al. Restoration of Toxoplasma gondii-specific immune responses in patients with AIDS starting HAART. AIDS. 2008;22:2087–96. [PubMed] 139.Fournier S, Rabian C, Alberti C, Carmagnat MV, Garin JF, Charron D, et al. Immune recovery under highly active antiretroviral therapy is associated with restoration of lymphocyte proliferation and interferon-gamma production in the presence of Toxoplasma gondii antigens. J Infect Dis. 2001;183:1586–91. [PubMed] 140.Venkataramana A, Pardo CA, McArthur JC, Kerr DA, Irani DN, Griffin JW, et al. Immune reconstitution inflammatory syndrome in the CNS of HIV-infected patients. Neurology. 2006;67:383–8. [PubMed] 141.Tremont-Lukats IW, Garciarena P, Juarbe R, El-Abassi RN. The immune inflammatory reconstitution syndrome and central nervous system toxoplasmosis. Ann Intern Med. 2009;150:656–7. [PubMed] 142.Desjeux P, Alvar J. Leishmania/HIV co-infections: epidemiology in Europe. Ann Trop Med Parasitol. 2003;97(Suppl 1):3–15. [PubMed] 143.Posada-Vergara MP, Lindoso JA, Tolezano JE, Pereira-Chioccola VL, Silva MV, Goto H. Tegumentary leishmaniasis as a manifestation of immune reconstitution inflammatory syndrome in 2 patients with AIDS. J Infect Dis. 2005;192:1819-22. [PubMed] 144.Sinha S, Fernández G, Kapila R, Lambert WC, Schwartz RA. Diffuse cutaneous leishmaniasis associated with the immune reconstitution inflammatory syndrome. Int J Dermatol.2008;47:1263-70. [PubMed] 145.Chrusciak-Talhari A, Ribeiro-Rodrigues R, Talhari C, Silva RM, Jr, Ferreira LC, Botileiro SF, et al. Tegumentary leishmaniasis as the cause of immune reconstitution inflammatory syndrome in a patient co-infected with human immunodeficiency virus and Leishmania guyanensis. Am J Trop Med Hyg.2009;81:559-64. [PubMed] 146.Neva FA. Biology and immunology of human strongyloidiasis. J Infect Dis. 1986;153:397–406. [PubMed] 147.Ridolfo AL, Gervasoni C, Antinori S, Pizzuto M, Santambrogio S, Trabattoni D, et al. Post-kala-azar dermal leishmaniasis during highly active antiretroviral therapy in an AIDS patient infected with Leishmania infantum. J Infect. 2000;40:199–202. [PubMed] 148.Gilad J, Borer A, Hallel-Halevy D, Riesenberg K, Alkan M, Schlaeffer F. Post-kala-azar dermal leishmaniasis manifesting after initiation of highly active anti-retroviral therapy in a patient with human immunodeficiency virus infection. Isr Med Assoc J. 2001;3:451–2. [PubMed] 149.Belay AD, Asafa Y, Mesure J, Davidson RN. Successful miltefosine treatment of post-kala-azar dermal leishmaniasis occurring during antiretroviral therapy. Ann Trop Med Parasitol. 2006;100:223–7. [PubMed] 150.Tadesse A, Hurissa Z. Leishmaniasis (PKDL) as a case of immune reconstitution inflammatory syndrome (IRIS) in HIV-positive patient after initiation of anti-retroviral therapy (ART) Ethiop Med J. 2009;47:77–9. [PubMed] 151.Gelanew T, Amogne W, Abebe T, Kuhls K, Hailu A, Schönian G. A clinical isolate of Leishmania donovani with ITS1 sequence polymorphism as a cause of para-kala-azar dermal leishmaniasis in an Ethiopian human immunodeficiency virus-positive patient on highly active antiretroviral therapy. Br J Dermatol.2010;163:870–4. [PubMed] 152.Kim AC, Lupatkin HC. Strongyloides stercoralis infection as a manifestation of immune restoration syndrome. Clin Infect Dis.2004;39:439-40. [PubMed] 153.Lanzafame M, Faggian F, Lattuada E, Antolini D, Vento S. Strongyloidiasis in an HIV-1-infected patient after highly active antiretroviral therapy-induced immune restoration [letter] J Infect Dis. 2005;191:1027. [PubMed] 154.Brown M, Miiro G, Nkurunziza P, Watera C, Quigley MA, Dunne DW, et al. Schistosoma mansoni, nematode infections, and progression to active tuberculosis among HIV-1-infected Ugandans. Am J Trop Med Hyg. 2006;74:819–25. [PubMed] 155.Taylor CL, Subbarao V, Gayed S, Ustianowski AP. Immune reconstitution syndrome to Strongyloides stercoralis infection. AIDS. 2007;21:649–50. [PubMed] 156.Plasencia LD, Socas Mdel M, Valls RA, Fernández EM, Higuera AC, Gutierrez AB. Terminal ileitis as a manifestation of immune reconstitution syndrome following HAART. AIDS. 2006;20:1903–5. [PubMed] 157.Shah I. Immune Reconstitution Syndrome in HIV-1 infected children - a study from India. Indian J Pediatr. 2011;78:540–3. [PubMed] 158.Subsai K, Kanoksri S, Siwaporn C, Helen L, Kanokporn O, Wantana P. Neurological complications in AIDS patients receiving HAART: a 2-year retrospective study. Eur J Neurol. 2006;13:233–9. [PubMed] 159.Auyeung P, French MA, Hollingsworth PN. Immune restoration disease associated with Leishmania donovani infection following antiretroviral therapy for HIV infection. J Microbiol Immunol Infect. 2010;43:74–6. [PubMed] 160.Blanche P, Gombert B, Rivoal O, Abad S, Salmon D, Brezin A. Uveitis due to Leishmania major as part of HAART-induced immune restitution syndrome in a patient with AIDS. Clin Infect Dis. 2002;34:1279–80. [PubMed] 161.Berry A, Abraham B, Dereure J, Pinzani V, Bastien P, Reynes J. Two case reports of symptomatic visceral leishmaniasis in AIDS patients concomitant with immune reconstitution due to antiretroviral therapy. Scand J Infect Dis. 2004;36:225–7. [PubMed] 162.Kérob D, Bouaziz JD, Sarfati C, Pavie J, Vignon-Pennamen MD, Menotti J, et al. First case of cutaneous reconstitution inflammatory syndrome associated with HIV infection and leishmaniasis. Clin Infect Dis. 2006;43:664–6. [PubMed] 163.Martin-Blondel G, Alvarez M, Delobel P, Uro-Coste E, Cuzin L, Cuvinciuc V, et al. Toxoplasmic encephalitis IRIS in HIV-infected patients: a case series and review of the literature. J Neurol Neurosurg Psychiatry. 2011;82:691–3. [PubMed] 164.Rodriguez-Rosado R, Soriano V, Dona C, González-Lahoz J. Opportunistic infections shortly after beginning highly active antiretroviral therapy. Antivir Ther. 1998;3:229-31. [PubMed] 165.Jiménez-Expósito MJ, Alonso-Villaverde C, Sardà P, Masana L. Visceral leishmaniasis in HIV-infected patients with non-detectable HIV-1 viral load after highly active antiretroviral therapy. AIDS. 1999;13:152-3. [PubMed] 166.González-Castillo J, Blanco F, Soriano V, Barreiro P, Concepción Bravo M, Jiménez-Nácher I, et al. Opportunistic episodes in patients infected with the human immunodeficiency virus during the first 6 months of HAART. Med Clin (Barc) 2001;117:81–4. [PubMed] 167.Javid B, Aliyu SH, Save VE, Carmichael AJ, Lever AM. Schistosomal colonic polyposis in an HIV-positive man. AIDS.2007;21:386–8. [PubMed] 168.Fernando R, Miller R. Immune reconstitution eosinophilia due to schistosomiasis. Sex Transm Infect. 2002;78:76. [PMC free article][PubMed] 169.de Silva S, Walsh J, Brown M. Symptomatic Schistosoma mansoni infection as an immune restoration phenomenon in a patient receiving antiretroviral therapy. Clin Infect Dis. 2006;42:303–4. [PubMed] 170.McCombe JA, Auer RN, Maingat FG, Houston S, Gill MJ, Power C. Neurologic immune reconstitution inflammatory syndrome in HIV/AIDS: outcome and epidemiology. Neurology. 2009;72:835-41. [PubMed] 171.Serpa JA, Moran A, Goodman JC, Giordano TP, White AC., Jr Neurocysticercosis in the HIV era: a case report and review of the literature. Am J Trop Med Hyg. 2007;77:113-7. [PubMed] 172.Albrecht H. Leishmaniosis-new perspectives on an underappreciated opportunistic infection. AIDS. 1998;12:2225-6. [PubMed] 173.Cabral RF, Valle Bahia PR, Gasparetto EL, Chimelli L. Immune reconstitution inflammatory syndrome and cerebral toxoplasmosis. AJNR Am J Neuroradiol.2010;31:E65–6. [PubMed] 174.Huruy K, Mulu A, Mengistu G, Shewa-Amare A, Akalu A, Kassu A, et al. Immune reconstitution inflammatory syndrome among HIV/AIDS patients during highly active antiretroviral therapy in Addis Ababa, Ethiopia. Jpn J Infect Dis. 2008;61:205–9. [PubMed] 175.Klotz SA, Aziz Mohammed A, Girmai Woldemichael M, Worku Mitku M, Handrich M. Immune reconstitution inflammatory syndrome in a resource-poor setting. J Int Assoc Physicians AIDS Care (Chic)2009;8:122-7. [PubMed]
Tệp đính kèm:
KSTHQ.doc
|

